
Dan Limmer, BS, NRP

by Dr. Bill Young
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
As the warm temperatures of summer settle in, the onset of anaphylaxis from bee stings and insect bites tends to increase. It’s important to know that these are not the main causes of anaphylaxis. It’s also key to know that, although related, allergic reactions and anaphylaxis are not the same disease processes. In this article, we will take a look at the pathophysiology behind anaphylaxis, as well as how it presents.
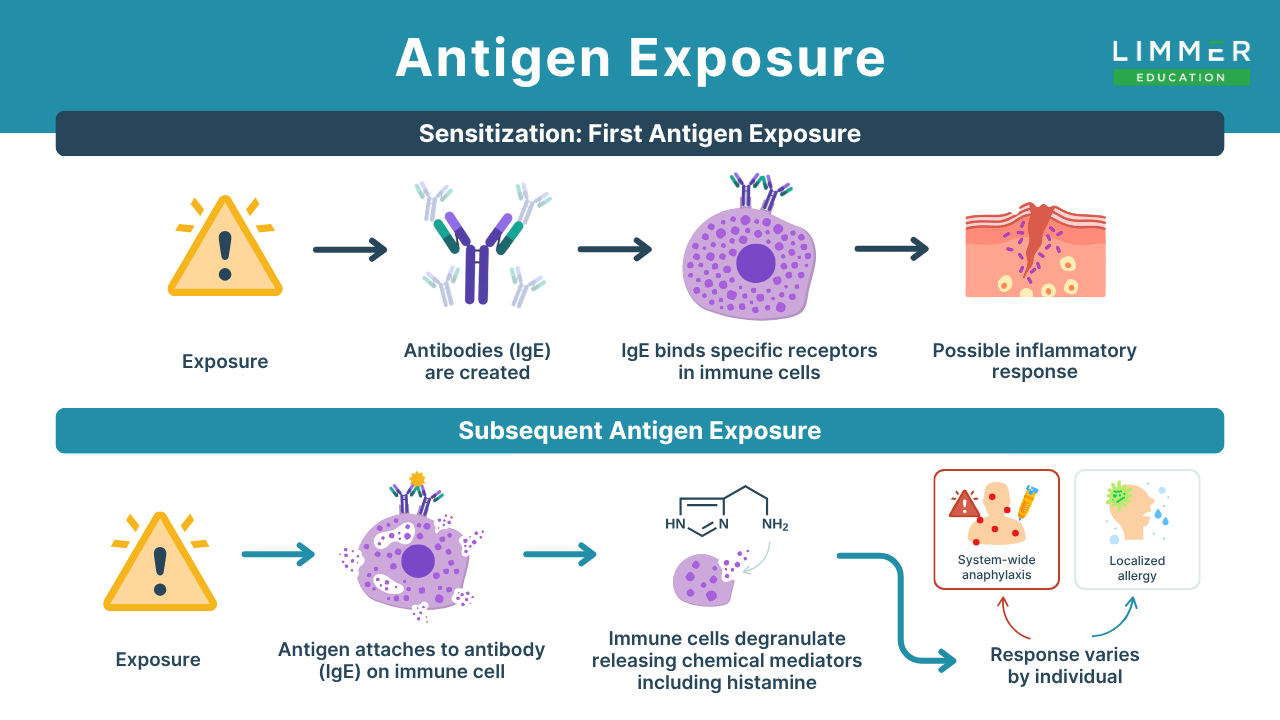
For the most part, anaphylaxis occurs when an antigen is injected into the body or introduced by way of the gastrointestinal system. When a person is first exposed to an antigen, there may be absolutely no reaction within the body. This initial interaction produces antibodies, but they remain in an inactive state until the same antigen is reintroduced into the body a second or third time. This early exposure may have a protective mechanism: Initial response causes the body to secrete a large amount of an antibody known as IgE. IgE binds specific receptors found on immune cells known as mast cells and basophils. These cells have a role in the inflammatory response that occurs early in an anaphylactic episode. With subsequent exposure, these cells undergo a process known as degranulation. Most histamine is produced by mast cells, as well as basophils of the white blood cell system. At the time of degranulation, they will release a large amount of histamine into the surrounding cells and tissues. Fun fact here: morphine has properties that can facilitate the release of histamine after being administered. The response depends upon the individual. It could be localized, thus being classified as an allergic reaction, or system-wide, the classic presentation of anaphylaxis.
Drug-induced anaphylaxis is common, with the rationale being that drugs injected into the body are rapidly absorbed into the central circulation and distributed widely throughout the body. The same happens when a patient sustains a bee sting. As a result of this allergen, the body begins to dump histamine and other chemicals that accompany the onset of anaphylaxis. The body systems primarily affected by anaphylaxis include the G.I. system, the skin, the respiratory system and the cardiovascular system.
The primary cause of death in patients with anaphylaxis is a combination of respiratory failure and distributive shock. The shock occurs from decreased vascular tone resulting from the release of histamine. Let's look at it in more detail.
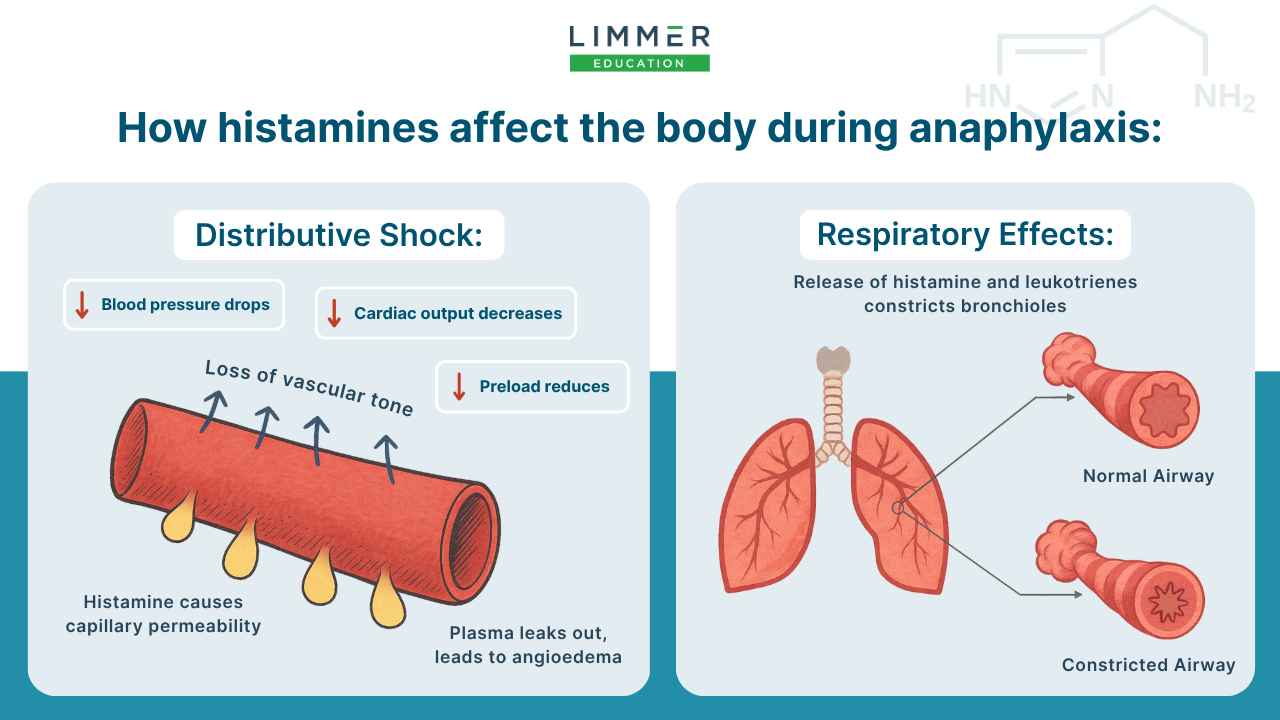
The mast cells of the body are the primary producers and releasers of histamine. This chemical causes the vasculature to dilate and become very permeable. The research shows that this vasodilation is probably caused by nitric oxide, which is released by the histamine. Nitric oxide’s effect on the body is vasodilation. It’s the same way nitroglycerin works during an acute coronary syndrome incident. It's almost as if someone took an ice pick to a firehose and put thousands of tiny holes in it. The result is a loss of fluid, in the form of plasma, and the ensuing drop in blood pressure ultimately causes circulatory collapse. The plasma leaks into the interstitial space. This causes preload to reduce. (Preload, as you recall, is the amount of blood delivered to the heart to be made available for oxygenation.) The result is a decrease in stroke volume and cardiac output. In addition, the leaking of plasma into the interstitial space leads to angioedema. One good thing about histamine release is that it is short-lived, because enzymes found within plasma almost immediately break down the histamine.
Bronchoconstrictors called leukotrienes cause a narrowing of the bronchioles, resulting in wheezing and increased vascular permeability. The body will produces leukotrienes on a normal basis, which helps maintain the homeostasis of constriction versus dilation of the bronchioles, but overproduction can result in disease processes such as asthma and those seen in anaphylaxis. The effect of leukotrienes is much longer than that of histamine.
So, what does the onset and progression of anaphylaxis look like? Your patient will probably present with signs and symptoms within 60 seconds of exposure to the allergen. Keep in mind that some patients may have a delayed reaction of up to an hour. Generally, the faster the onset of symptoms, the more severe the reaction. This is one of those times when the old saying “speed kills” is often true.
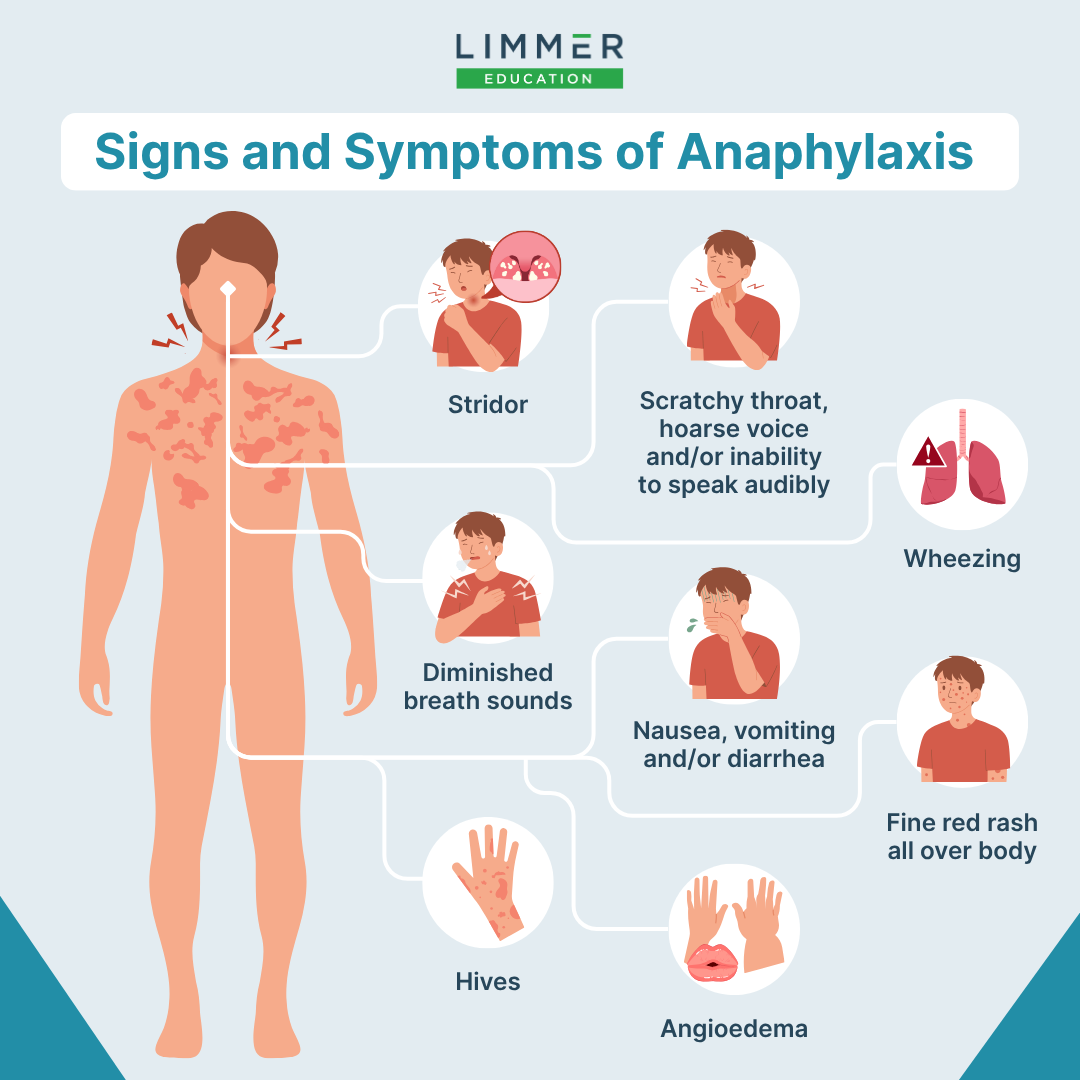
As with all patients, it is imperative to rapidly and accurately assess a patient having an anaphylactic episode. One of the first symptoms your patient will have is feeling a sense of impending doom. This is largely due to the hypotension caused by vascular permeability, as well as the reduction in the amount of oxygen being delivered to the brain cells. Be aware of problems with the patient's airway, especially the upper airway. These patients can present with edema of the larynx, which may prevent them from being able to speak audibly. This can often present as a patient complaining of a scratchy throat and a hoarse voice. Unaddressed, the patient will soon have symptoms of stridor and then respiratory collapse. As the hypotension and hypoxia continue to worsen, the patient will often become restless and even combative. If the symptoms are not immediately addressed, the patient will progress to unresponsiveness. Breath sounds will often be diminished or not heard at all, depending on how tight the bronchoconstriction is in the lungs.
One of the key markers in a patient with anaphylaxis is an early change in skin condition. Patient will often have a very fine red rash that is spread all over the body, with special concentration within the area of the point of injection. As histamine continues to be released, urticaria, also known as hives, begin to appear. Hives are large, red, raised bumps that can appear and disappear suddenly. Angioedema is caused by plasma leaking out of the vasculature because of histamine’s effect on that system.
Because of the increased motility of the gastrointestinal system, you may hear hyperactive bowel sounds when you listen there. This happens because of an increase in the smooth muscle contraction of the gut. It is often accompanied by nausea, vomiting and diarrhea. This contributes to making the hypovolemic shock worse.
In conclusion, understanding the pathophysiology of anaphylaxis is crucial for promptly recognizing and effectively managing this life-threatening condition. Paramedics and healthcare providers must be able to:
Distinguish between allergic reactions and anaphylaxis.
Comprehend the underlying mechanisms—such as IgE-mediated mast cell degranulation and the subsequent release of histamine and leukotrienes.
Rapid assessment and intervention are paramount, as the progression can occur swiftly. Ultimately, diagnosis and treatment of anaphylaxis not only saves lives but also enhances the quality of care provided in emergency settings.
Dr. Bill Young is an Associate Professor in the Emergency Medical Care program at Eastern Kentucky University and host of the Ten Minute Medic podcast. He has worked in emergency medical services since 1978. He began his career running calls for a small fire department near Williamsburg, Kentucky long before the term “first responder” existed. Young has worked as a street medic, training officer, supervisor, state regulator and educator.

Dan Limmer, BS, NRP

Dan Limmer, BS, NRP