Back to the Basics: Burns

by Chris Ebright
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
“Anything will burn with enough gasoline and dynamite.” - Robert Heinlein
When a patient is severely burned, it changes their life. Not only in that moment, but for years to come. Annually, over two million people in the U.S. are treated for burns, and fortunately, the majority are not considered life threatening. However, EMS professionals are likely to come across a patient that requires major burn care sometime in their career. What is done for that patient in the first minutes can make a difference between a positive or a negative long-term outcome.
Pathophysiology of Burns
The skin is made up of three distinct layers: the epidermis, dermis, and hypodermis/subcutaneous. As a burn progresses through each subsequent layer, the consequences become more debilitating. The depth of the burn depends upon how long the patient was in contact with the heat source, the thickness of the patient’s dermis, and the temperature of the source. Regardless, with any type of burn the barrier that repels microorganisms, assists in thermoregulation, maintains fluid and electrolyte balance, and processes pain, touch, heat and cold is compromised.
When heat is applied to the skin, it denatures its protein structure. This essentially disrupts the skin’s molecular configuration and, in some cases, forever alters it. At the point of contact, and within the surrounding tissue, three distinct areas develop. The first is the zone of coagulation. The maximum amount of damage occurs here and irreversible tissue loss, due to protein destruction, results. The zone of stasis is the area surrounding the zone of coagulation. It is the area of skin beneath the coagulated surface of a burn in which blood flow is diminished and tissue fluid collects. This region of a burn may become necrotic if it becomes infected or fails to receive adequate blood flow. On the outermost edge of the burn is the zone of hyperemia. Here, tissue perfusion is adequate due to patent blood vessels, and erythema occurs due to increased vascular permeability. The tissue will usually recover unless there is severe sepsis or prolonged hypoperfusion.
Eventually with deep burns involving the dermis and hypodermis, capillaries within the affected area dilate. This increased capillary permeability allows an extraordinary amount of plasma to leak from the blood vessels into the surrounding tissue. Tissue edema and vascular hypovolemia results. Typically, if the burn surface area is 20% or greater, an increase in blood viscosity, electrolyte imbalances, and reduced cardiac output may result. Fortunately, it takes hours to manifest, but understanding this should make the EMS professional aware that early fluid replacement is essential.
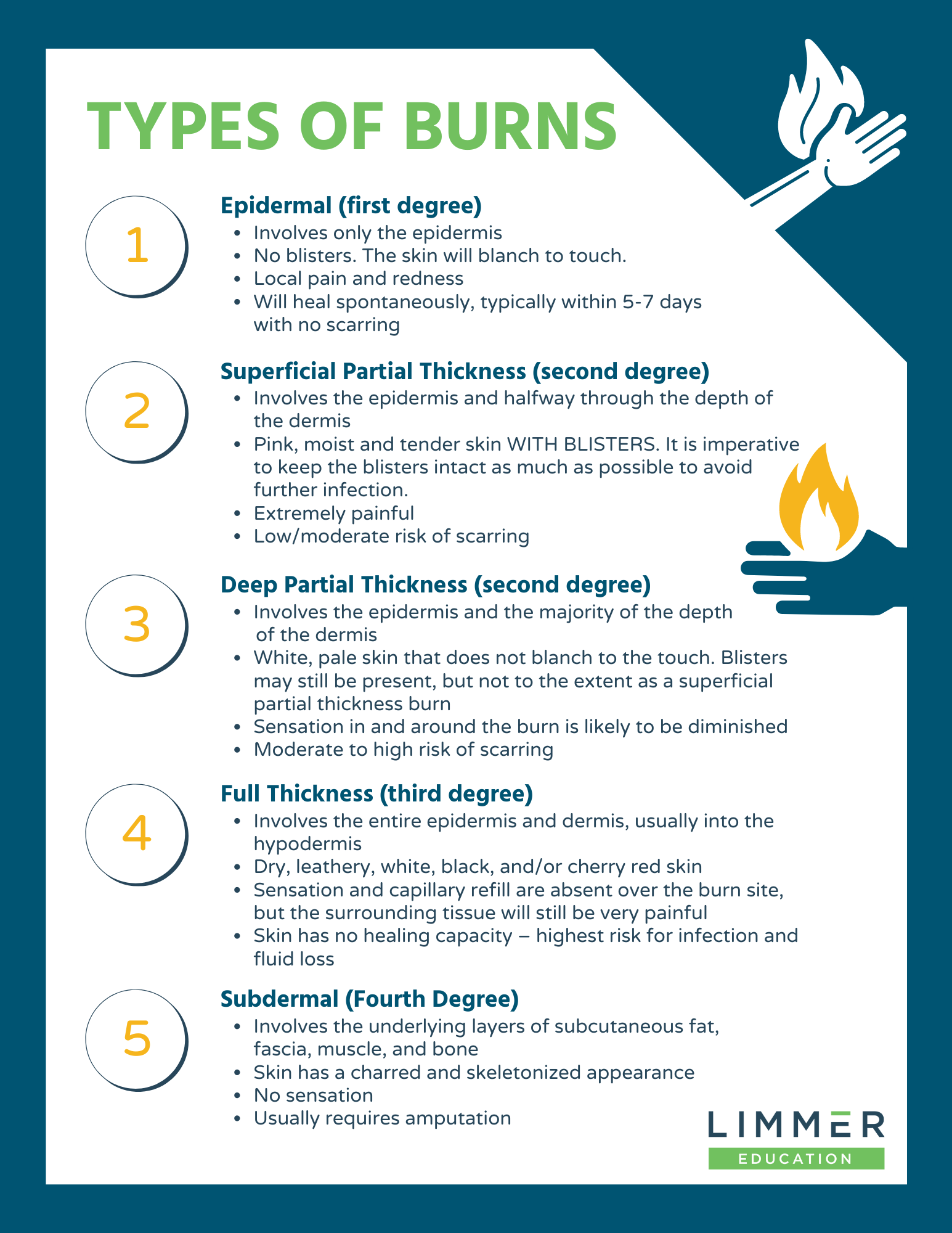
Types of Burns
The severity of a burn injury is determined primarily by body surface area involved and not so much the depth of the burn. However, both should be considered when assessing a patient.
Epidermal (first degree)
Involves only the epidermis
No blisters. The skin will blanch to touch.
Local pain and redness
Will heal spontaneously, typically within 5-7 days with no scarring
Superficial Partial Thickness (second degree)
Involves the epidermis and halfway through the depth of the dermis
Pink, moist and tender skin WITH BLISTERS. It is imperative to keep the blisters intact as much as possible to avoid further infection.
Extremely painful
Low/moderate risk of scarring
Deep Partial Thickness (second degree)
Involves the epidermis and the majority of the depth of the dermis
White, pale skin that does not blanch to the touch. Blisters may still be present, but not to the extent as a superficial partial thickness burn
Sensation in and around the burn is likely to be diminished
Moderate to high risk of scarring
Full Thickness (third degree)
Involves the entire epidermis and dermis, usually into the hypodermis
Dry, leathery, white, black, and/or cherry red skin
Sensation and capillary refill are absent over the burn site, but the surrounding tissue will still be very painful
Skin has no healing capacity – highest risk for infection and fluid loss
Subdermal (Fourth Degree)
Involves the underlying layers of subcutaneous fat, fascia, muscle, and bone
Skin has a charred and skeletonized appearance
No sensation
Usually requires amputation
Any combination of the above may be present during assessment. Most commonly, thermal injuries are the culprit when EMS responds to assist a burn patient. Scalds from spilling hot drinks or liquids, or being exposed to hot bath water tend to cause superficial / superficial partial thickness burns. These occur in a majority of burns involving children and the elderly. Fifty percent of adult burns result from flame injury, and often are associated with inhalation and other traumatic injuries. They tend to be deep partial thickness or full thickness burns.
General management revolves around stopping the burning process. Remove clothing, jewelry, metal, or anything else that can retain and/or conduct heat. If any material is adhered to the skin, stop the burning process by cooling the material, cutting around it, and removing as much as possible. With smaller size injuries (typically ≤5% BSA) cool the burn briefly with water. Be aware that prolonged application of cold poses the risk of wound and systemic hypothermia. Wound hypothermia reduces blood flow to the damaged area and may deepen the injury. Cover the affected area(s) and the patient with clean, dry sheets. Analgesia for small surface area burns can be accomplished with saline-soaked gauze. Wet, cool dressings feel better, and there is very little likelihood of developing hypothermia. Once the burning process is stopped, transition to a dry, loose dressing. Moderate to severe surface area and deep burns likely require opioids or similar analgesia. Be sure to administer your medication of choice only via intravenous route, and in a dose enough to control pain.
Electrical injury is another mechanism, and the sources vary considerably. The alternating nature of household current tends to be low voltage, but still can cause relatively deep contact burns and possible arrhythmias. The polar opposite are tension wire injuries, where the voltage is monumentally higher. Contact usually results in catastrophic muscle and organ damage, amputation, and fatal outcomes. Flash/Splash injuries from lightning are less common, but potentially dangerous as clothing can be set alight, resulting in widespread body surface burns. Additionally, with a “flashover effect,” the shower of electricity may find its way into the body through an orifice. Once inside, electricity travels through tissue with the least amount of resistance - nerves and blood vessels. As a result, any body system has the potential to be affected. This should keep your index of injury suspicion very high until the patient is delivered to the hospital. Along with standard burn care, ECG monitoring is essential.
Industrial accidents and household chemical products also cause varying degrees of burns. Acids and alkalis are common culprits, with burns that tend to be deeper in general, due to their corrosive nature. An alkali tends to liquefy tissue as it burns. Acids tend to cause an almost instant protein coagulation; thus, the depth of burn tends to be smaller in comparison. Regardless of the source and appearance of a chemical burn, copious irrigation is essential. Patients exposed to hydrofluoric acid, which is used in glass etching and circuit board manufacturing, may require additional support with calcium gluconate gel applied to the burn. Dry chemicals should be brushed off prior to irrigation. Other chemicals that react with water, such as sodium metal, should be brushed off then covered with an oil-based dressing. Tar and asphalt burns should be thoroughly cooled with copious amounts of water.
Burns Assessment and Management
Keep in mind that there may be other associated traumatic injuries with burn patients. It will be important to manage the burn but that may be secondary to other, more pressing, needs of the patient. Airway compromise – especially with thermal burns – is one real possibility. Inhalation of superheated air or steam causes swelling to upper and lower airway structures, compromising ventilation. Look for evidence, such as: changes in voice, wheezing, or other adventitious sounds such as stridor or a brassy cough; singed nasal hairs and/or eyebrows; facial burns; soot in the sputum and/or around the mouth or nose; or, a progressive decline in level of consciousness – agitation, anxiety, disorientation, obtunded, unconsciousness.
Depending on the thermal source, toxin inhalation of gasses from ignition of plastics and other synthetics must be considered. You may have to manage an anatomical airway issue but also the physiological effects of byproducts such as cyanide and carbon monoxide. These tend to be a more frequent airway/oxygenation complication than the thermal inhalation burn. Oxygenate and/or ventilate the patient, as needed, with high-flow oxygen. Consider early advanced airway management and antidote therapy with specific cases: hyperbaric chamber for severe carbon monoxide poisoning; cyanide reversal agents such as nitrite and thiosulfate or Hydroxocobalamin (Cyanokit).
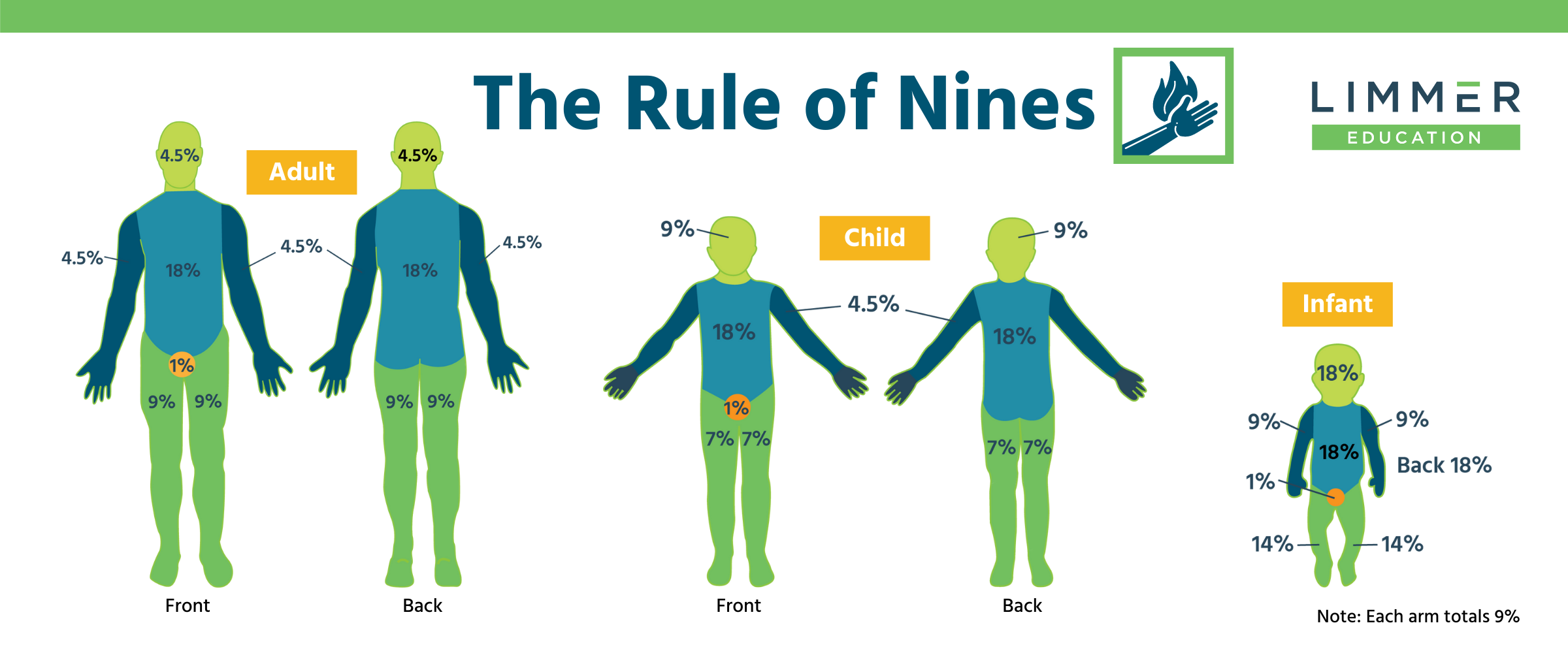
As mentioned previously, the severity of a burn injury is determined primarily by body surface area (BSA) involved and not so much the depth of the burn. The most common method to calculate burned BSA is the “Rule of Nines.” This is typically used if more than ten percent BSA is involved. If the area is less than ten percent, the size of the patient’s hand, including the fingers, can be used as a guideline. It represents one percent BSA. It is important to note: only second and third degree total burn surface areas are used to calculate using Rule of Nines. First-degree burns should not be included in the fluid resuscitation calculations as it increases the likelihood of over-resuscitation.
Having done your best to calculate BSA involved, take one step back before you continue your management. Scan the body for obvious fractures and uncontrolled bleeding. Check for circumferential burns around the arms and/or legs, especially deeper partial thickness and full thickness. If present, compartment syndrome may develop. Immobilize the limb(s) and check them frequently, reassessing distal pulse, sensation, and movement. Note any progressive deterioration and radio your findings as early as possible. If a deeper burn is circumferential to the chest/thorax, it likely will compromise the patient’s ability to ventilate. This will require aggressive airway and ventilatory measures until the patient can be delivered to the hospital. Once in the ED, an escharotomy will be performed in both cases to restore perfusion / allow the chest to expand.
What about fluid? Resuscitation fluid needs are related to the extent of the burn and patient body size. Patient age further influences the relationship of fluid needs to body size, since children have nearly three times the BSA to body mass ratio, compared to adults. Administering IV fluid early to burned patients helps provide a buffer/reservoir for the eventual fluid shift, as mentioned earlier. Using Lactated Ringer’s as the preferred fluid, per the American Burn Association, the current formulas for burn resuscitation are:
Adults: 2 ml (x) kg body weight (x) BSA burned
Children: 3 ml (x) kg body weight (x) BSA burned
Using these guidelines ensures sufficient fluid replacement, while preventing over-hydration. Administer half of the calculated dose in the first 8 hours and the second half over a remaining 16 hours. In essence, you are giving enough reserve fluid volume to make up for when the capillary permeability and fluid shift is the highest.
Burn Centers
Transporting a burn patient to the proper facility is just as important as good field management. Burn centers are staffed by experts in the care of burn patients and provide the best possibility for recovery and long-term wellness. There may not be a center in close proximity to your scene, in which case, the patient should be transported to a high-level trauma center. The staff will be able to stabilize most burn patients, and then decide when and if to refer the patient to a burn center. Protocols vary, but in general, burn injuries that should be referred to a burn center include:
Partial thickness burns greater than 10% total body surface area (TBSA)
Burns that involve the face, hands, feet, genitalia, perineum, or major joints
Third degree burns in any age group
Electrical burns, including lightning injury
Chemical burns
Inhalation injury
Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality
Any patient with burns and concomitant trauma (such as fractures) in which the burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, the patient may be initially stabilized in a trauma center before being transferred to a burn unit.
Burned children in hospitals without qualified personnel or equipment for the care of children.
Conclusion
Most burn injuries are not life-altering, but others can be devastating. Effective prehospital care is an important step in maximizing the best possible outcome for all burn patients. Always be prepared to rapidly assess burn severity and surface area, aggressively manage an airway, stop the burning process, prevent hypothermia, and fluid resuscitate early.
References
Hero Burn Foundation. (2019, February 5). Depth of Burn #beburnaware. [Facebook Post]. Facebook.
Guidelines for the Operation of Burn Centers (pp. 79-86), Resources for Optimal Care of the Injured Patient 2006, Committee on Trauma, American College of Surgeons
zone of stasis. (n.d.) Medical Dictionary. (2009). Retrieved October 23, 2021.
Burn Care in EMS. EMS World. (2004, February). Retrieved October 26, 2021, from burn care in EMS.
Related articles

Dan Limmer, BS, NRP

Dan Limmer, BS, NRP
Comments
Leave a commentThanks for the notes am fully satisfied