
Limmer Education

by Limmer Education
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
A new position paper on spinal motion restriction (SMR) was issued by the American College of Surgeons (ACS), American College of Emergency Physicians (ACEP), and the National Association of EMS Physicians (NAEMSP). It is another in a series of position papers on the topic and it may be the best yet on the subject. It can be found here.
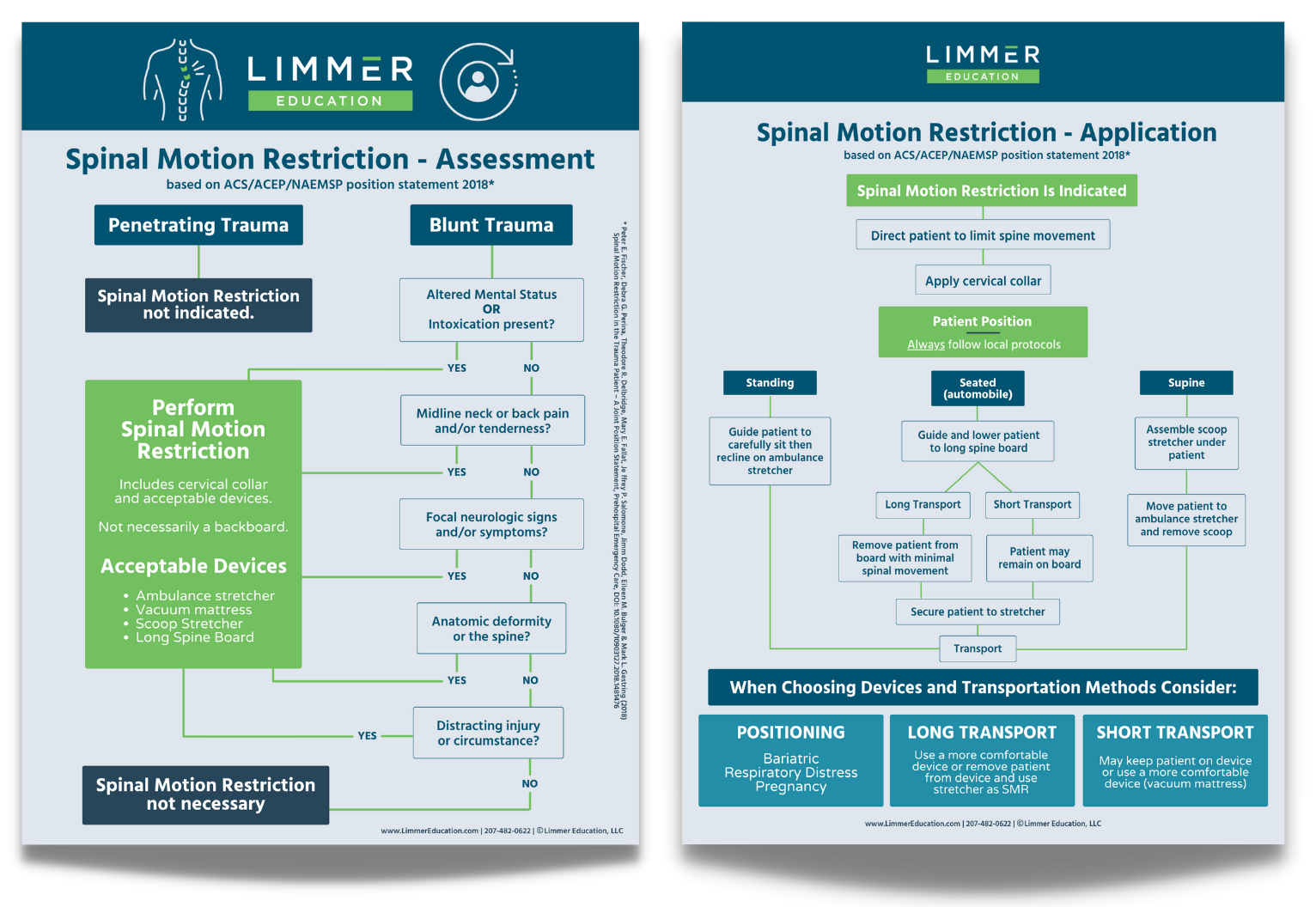
The position paper answers questions many have had about what devices are acceptable and how and when they should be used. This should help with leveling the playing field on a topic that has been in a state of flux for some time. We’ve created a flowchart to help teach your students about SMR.
Download the flowchart (PDF) or purchase the poster set for your classroom.
The position paper makes some helpful statements. Here are some highlights and the teaching implications for each.
Position Paper Statement | Teaching Points |
|---|---|
5 elements of spinal assessment | • Teach these in class. • Discuss why each of these are important. • Practice spinal assessment in class during the assessment module. |
There are options for spinal motion restriction | • Avoid talking about the old days when everyone went on a backboard! • Give your students different patient presentations or scenarios where certain devices would be better (difficulty breathing, bariatric patients, pregnant patients) and let them decide. |
The position paper gives some guidelines on when to remove the patient from a device to the stretcher (short vs long transport). | • Have students develop definitions for short and long transport time. Help them with criteria (need for motion restriction, comfort, injury type(s), etc.). Use local transport times and locations for reality. |
The paper notes that movement to and from a device is the point when unstable injuries are most vulnerable. | • Practice moving patients to SMR devices as well as from devices onto the stretcher with minimal movement. |
Note the specific pediatric recommendations that are different than for adults. | • It is always good to discuss pediatric issues. Since peds patients may not always be able to tell you what is wrong. It is acceptable to bring in MOI and extent/location of injuries in making a decision about SMR. • Torticollis is a term you and your students should know. |
As for the “Will the NREMT be testing these positions now?” question, it’s safe to say that this position paper is more of a practical refinement than a “new skill” situation, and it will fit in relatively well with the current NREMT examinations.
What do you think of the new position paper? How will you integrate it into your education and practice?
Buy the SMR poster set for your classroom!

Limmer Education

Limmer Education

Dan Limmer, BS, NRP