
Limmer Education

by Chris Ebright
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
Unintentional injury is the leading cause of death and disability in children, more than all other causes combined.
These injuries result in over nine million emergency department visits per year, of which over twelve thousand conclude with a child's death. Depending on age, the primary cause of death varies. Two-thirds of the cases involving children less than one year old typically are due to suffocation. Drowning is the leading cause of traumatic death for children one to four years old. Lastly, with children five to nineteen years old, most injury deaths involve being an occupant of a motor vehicle traffic crash.
Severely injured children ideally should be transported to a facility staffed 24/7 by personnel experienced in child trauma. However, EMS professionals must consider the unique pediatric trauma victims' anatomy and physiology during the interim treatment and transport. How do these differences from adults influence the findings during a trauma assessment and then dictate the ensuing management? Let's take a closer look.
Consider the possibility of serious injury if any of the following are present during an assessment:
There is a significant mechanism of injury, regardless of obvious injuries.
The injured child has an altered mental status or is behaving inappropriately.
The injured child has evidence of poor systemic perfusion.
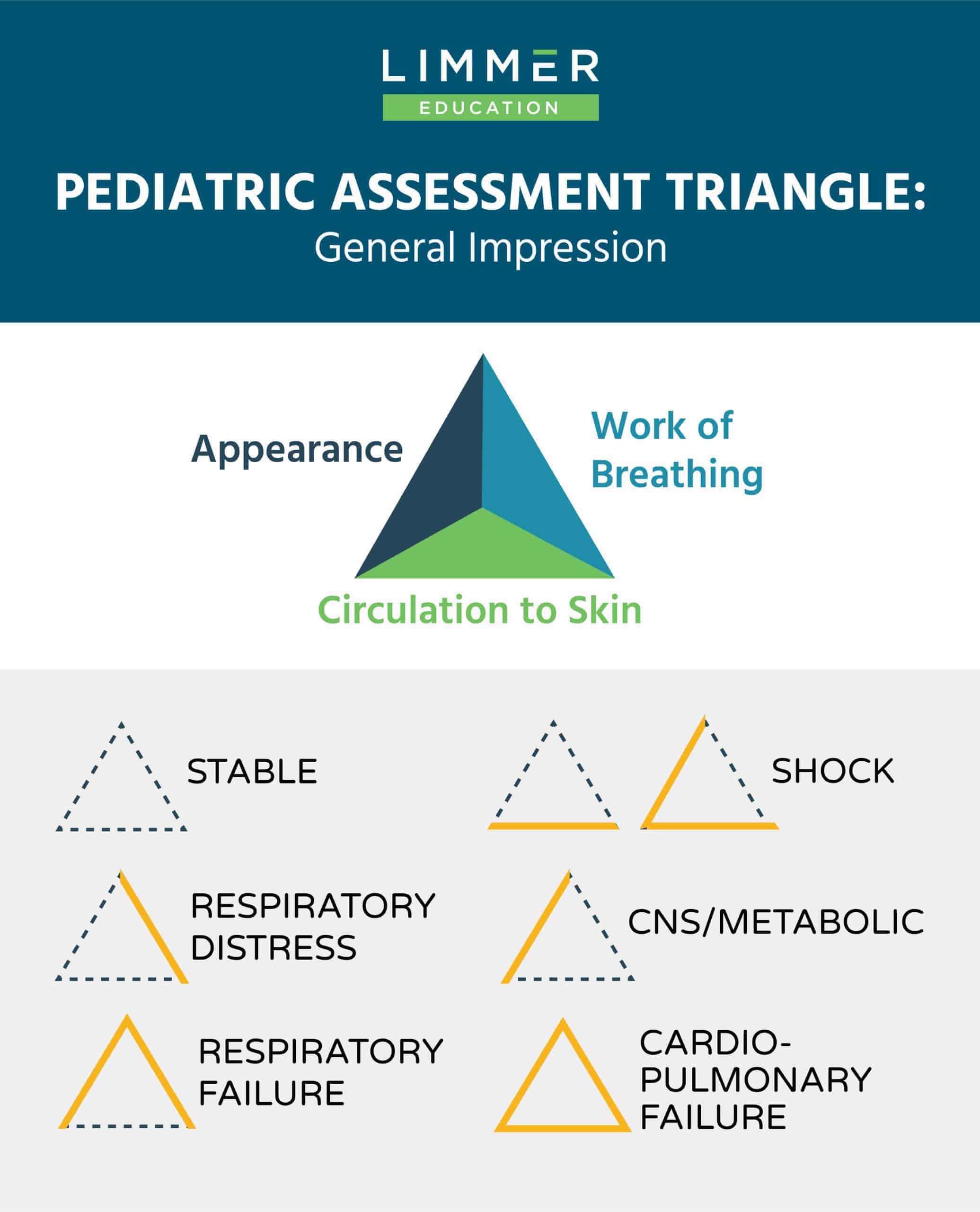
Additionally, by visually assessing the patient, it is likely you may be able to determine their current physiological status by using the Pediatric Assessment Triangle.
While spinal cord involvement is rare (<2% of injured children), a mismanaged underlying injury may have devastating consequences. Motor vehicle crash is typically the primary culprit, resulting in a cervical vertebrae subluxation or distraction injury; due to a child's large head and relatively weaker neck. Since these smaller patients' necks are so small, it is also hard to palpate or visualize any deficit. Thus, all significantly injured children have a cervical vertebral injury as a rule of thumb until proven otherwise - precluding any head-tilt maneuvers. Moreover, in-line cervical stabilization is essential throughout any intubation attempt, basic or alternative (LMA/iGel) airway insertion, or during BVM ventilation. Secondary to their primal anatomy, these procedures have a natural, but with a trauma patient - significant, effect on a pediatric cervical spine. Depending on the intervention, anterior/posterior vertebral displacement, increased pressure on the spinal column, widening of the intervertebral disk space, or an extension of the articulation between C1 and the skull can worsen a patient's condition.
Obstruction of the airway can occur anywhere between the lips and the carina - by direct trauma, edema, secretions, blood, or stomach contents. It is smaller in width and length when compared to an adult, increasing (among other things) the risk of obstruction with foreign bodies. Additionally, a relatively small amount of edema (burns, especially) can significantly reduce airway diameter and patency.
An infant's occiput is proportionally larger than a child's, and a child's occiput is larger than an adolescent/adult. The result is a flexed head when supine. Since a pediatric trachea is more flexible than the typical adult's, any amount of hyperflexion or hyperextension can create a partial or total airway occlusion. Sufficiently padding under the child to achieve a neutral alignment position easily remedies this complication.
Infants and children proportionally have a larger tongue, a wider epiglottis, and a smaller oropharynx. These patients also have a superior and anterior larynx (typically sitting at the level of C2-C3). These differences can contribute to a partial or total airway obstruction – especially when a pediatric patient is positioned supine. Take extreme care when placing an airway adjunct, and make sure it is the proper size. It can directly obstruct the glottic opening or displace the tongue and epiglottis posteriorly, effectively doing the same thing if it is too large.
Lastly, newborns, neonates, infants, and (to an extent) toddlers are obligate nose-breathers. This means that their brain only recognizes that their nares and not their oral cavity are a means to inhale and exhale. Thus, when blood or a nasal deformity from facial trauma is present, it may effectively block their airway. Proper lateral positioning and suctioning should resolve any presenting signs of airway obstruction or poor ventilation. If using a bulb syringe, be sure to squeeze it before insertion.
Any head, face, or neck trauma with associated altered mental status is a dangerous situation. Manage the pediatric airway immediately, as these patients cannot effectively protect the upper airway. The concomitant depressed gag reflex can allow the patient to aspirate and create a lower airway compromise.
If an airway issue is not impeding proper ventilation, the culprit may lie in the ability to ventilate. Hypoventilation secondary to thoracic trauma inevitably induces hypoxia, which is the number one cause of cardiac arrest in infants and children. Anatomically, the thoracic organs are in much closer proximity. Thus, an injury that appears minor or one-sided on the chest may have created extensive internal damage.
A child's ribs are positioned horizontally. Consequently, during inspiration, the ribs only move up and not up-and-out like an adult rib cage. This lack of expansion reduces the pediatric patients' ability to increase tidal volume effectively. Any type of chest injury will likely exacerbate this limitation, and as such, assisted ventilation (even with what seems minor trauma) may be necessary.
Pediatric total blood volume averages between 80 and 90 ml/kg. Therefore, what appears to be a relatively small external blood loss is still very significant. For example, a 50 ml hemorrhage experienced by a 5 kg child represents a loss of approximately 10% of his/her total blood volume. Thus it goes without saying, external hemorrhage requires immediate management. When treating a pediatric trauma patient, it may likely be your initial intervention, even before airway. Direct pressure will usually do the trick, but do not be afraid to utilize tourniquets and possibly hemostatic agents if needed.
Children vasoconstrict more efficiently and proportionally longer than an adult. This allows a 25-30% loss of their blood volume before signs of shock appear. During assessment, this physiologic response makes the compensating patient appear to "not look too bad." However, keep this in mind: children cannot increase myocardial contractility - they maintain cardiac output by increasing heart rate. When assessing a pediatric trauma patient, look for persistent tachycardia. It is the earliest and most reliable indicator of shock in a child.
Another very reliable sign of volume deficit is delayed capillary refill. The vasoconstriction, as mentioned earlier, will initially target the extremities, producing a blanching delay, despite a relatively normal overall skin color.
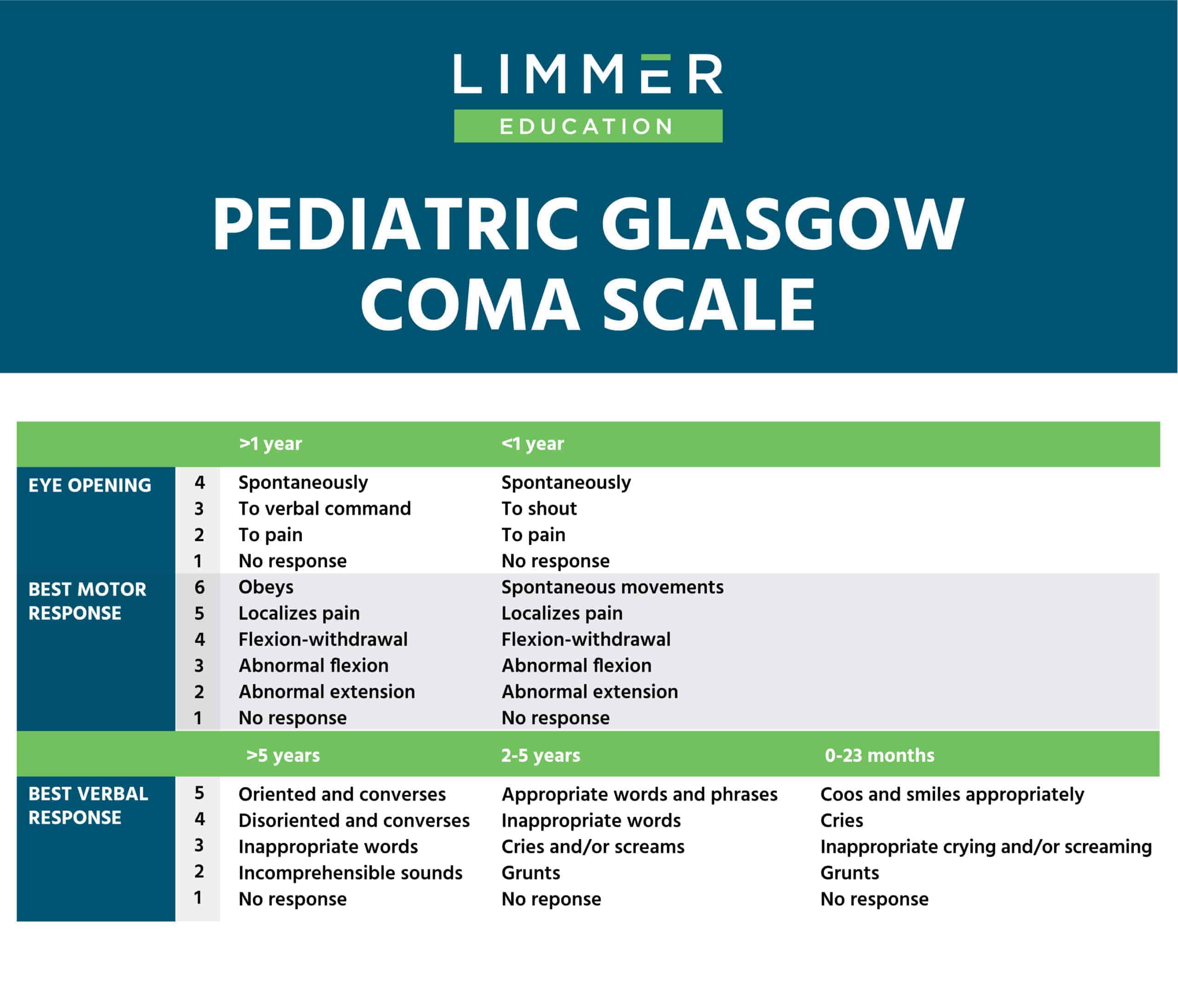
This is usually a good time to pull up a pediatric trauma app or another reliable reference to help establish a baseline Glasgow Coma Scale. Check and see if the patient is awake or not. Can s/he follow commands? Do they move their extremities voluntarily or require some type of stimulation?
Make sure that the responder that does the initial assessment is the one to reassess as well. This will help to avoid any differences in perception and maintain the consistency of the exam.
A child's body surface area to body mass ratio, compared to adults, is much higher. Coupled with faster ventilation rates, they expel body heat proportionally faster. With any amount of volume loss, acceleration of heat loss is also inevitable. As such, all pediatric trauma patients have a high risk of developing hypothermia, even on the warmest of days. If left unchecked, the concomitant arrhythmias, coagulation abnormalities, and acidosis worsen their condition.
Cranial sutures and fontanelles remain open through eighteen months of life. This allows for temporary pressure release in the setting of brain swelling or intracranial bleeding, but by its nature, it decreases cranial stability. Additionally, a child's cranial bones do not afford as much protection - they are thinner than an adult.
The infant or child's head is proportionally larger, producing a natural high center of gravity. This predisposes them to falling and sustaining head and/or neck trauma, even a minor distance.
A weaker connection exists between the subdural & subarachnoid layers of the meninges. Coupled with proportionally high water content, the pediatric brain has a higher incidence of coup and contrecoup injuries, axonal shearing, intracranial, and intracerebral bleeding from blunt traumatic forces.
Airbags can be another significant contributor to a pediatric patient's poor outcome. State laws vary, but there are reasons that children are placed in the back seat facing backward and then eventually forward, in proper car seats.
Their short stature puts their head at or near the level of the passenger airbag. Once it deploys, it either will directly strike the head or force the car seat into the passenger seat, crushing the infant or child's head.
Their immature neck musculature coupled with flatter occipital condyles creates the potential for subluxation or hyperextension of the cervical spine from a direct facial impact. Both of which can lead to a partial internal or external decapitation.
The airbag impact striking the face may result in a multitude of facial, nasal, orbital, and/or mandibular fractures – increasing the difficulty of managing the pediatric patient's airway.
A pediatric rib cage is more pliable, with a proportionally lesser amount of subcutaneous fat and chest muscle mass. As a result, kinetic energy associated with blunt chest trauma has far less resistance passing into a child's body compared to an adult. Pulmonary contusion (the most common intrathoracic injury), tension pneumothorax, and hemothorax are likely with what appears to be minor chest trauma. Keep in mind that any of these injuries cause a ventilation/perfusion mismatch. Management of the imminent hypoxemia and hypoxia will be at a premium during your patient encounter.
Blunt chest trauma may also result in a higher incidence of cardiac tamponade with pediatric trauma patients due to the anatomical difference explained above. Additionally, Commotio Cordis (an instantaneous cardiac arrest produced by a non-penetrating blow to the chest) may be the origin of a pediatric trauma call. Typically, this occurs from blunt impact to the left chest in the neighborhood of the third to fifth intercostal space by an object traveling at least 30 miles per hour. The object can be anything from a fist punch, a line drive from a baseball, the heel of a hockey stick, or leading with the helmet during a football tackle.
Abdominal trauma is the most common cause of unrecognized fatal injury in children. Children have proportionally larger solid organs, less subcutaneous fat, and less protective abdominal musculature than adults do. As a result, they suffer relatively more solid organ injury from both blunt and penetrating mechanisms. Bicycle handlebars are a common cause of blunt abdominal trauma, with the spleen being the most commonly injured organ.
Consider this the case during an assessment if you discover:
Trauma to left thorax or abdomen
Signs or symptoms of shock
Complaint of left shoulder pain after abdominal trauma
Noted lower rib fractures

Approximately one-third of children will have significant intra-peritoneal injuries from blunt abdominal trauma related to motor vehicle crashes. Typically, inappropriate seatbelt use is a major factor, causing lumbar vertebral, bowel, stomach, pancreatic, and mesenteric injuries. These can occur with a lap belt alone or with a three-point restraint. Termed seatbelt syndrome, many children are predisposed because their feet do not reach the floorboard, and they tend to slouch.
Additionally, due to their height, the lap belt improperly crosses over the abdomen at their umbilicus rather than the iliac crests of the pelvis. During a frontal MVC, upon impact, the seat belt locks and pulls a patient backward at the navel region. The resultant excessive flexion of the spine causes a Chance Fracture in the lumbar region. As the patient bends forward, it is very likely he or she also hits their head on the back of the front seat, possibly causing a cervical spine injury. If they are in the front seat, injuries are likely from contact with the airbag.
Most extremity injuries are not going to kill your pediatric patient. If anything, they will be a primary source of pain, which may either exacerbate other injuries or muddle your trauma assessment. Keep in mind that children's bones are more flexible than those of an adult. The old adage "kids bounce, not break" stems from the fact that a vast majority of their skeletal matrix is still cartilage. As a result, most injuries are greenstick-type fractures. However, one may encounter a complete fracture that has a significant deformity. Injuries involving the femur or pelvis not only have the potential for high volume blood loss, but one must also consider the nature of the bone structure. It took a tremendous amount of force to fracture these "flexible" structures. As mentioned earlier, that associated kinetic energy easily transfers internally and can cause additional injuries throughout the body. Remember, the smaller the child, the closer the organs are packed together.
In conclusion, when blunt and penetrating forces impact a child's body, multisystem trauma frequently occurs. Although most injuries are mild or moderate in severity, the EMS professional should be prepared to evaluate and manage pediatric trauma patients rapidly. Additionally, children have differing anatomy and physiology from adults, which requires specific attention during their assessment and management. If there is any patient deterioration at any time, the initial assessment should be repeated and any newly identified problems addressed. Definitive management by a pediatric trauma surgeon at a pediatric trauma center, whenever possible, is optimal to ensure the best patient outcome.
McFadyen JG, Ramaiah R, Bhananker SM. Initial assessment and management of pediatric trauma patients. Int J Crit Illn Inj Sci. 2012;2(3):121-127. doi:10.4103/2229-5151.100888.
Smyth BT. Chest trauma in children. J Pediatr Surg. 1979;14:41–7.
https://www.orthobullets.com/pediatrics/4124/pediatric-trauma-evaluation-and-management
Prusakowski MK1, Chen AP2. Pediatric Sepsis. Emerg Med Clin North 2017 Feb;35(1):123-138.
Link MS, Estes NA. Athletes and arrhythmias. J Cardiovasc Electrophysiol. 2010; 21:1184–1189.
Nadler EP, Potoka DA, Shultz BL, Morrison KE, Ford HR, Gaines BA. The high morbidity associated with handlebar injuries in children. J Trauma. 2005;58:1171–4.
Stafford PW, Blinman TA, Nance ML. Practical points in evaluation and resuscitation of the injured child. Surg Clin North Am. 2002;82:273–301.
Das, Joe & Sapkota, Rashmi & Shrestha, Binjura. (2018). Pediatric dural venous sinus thrombosis following closed head injury: an easily overlooked diagnosis with devastating consequences. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery: TJTES. 24. 74-77.

Limmer Education

Limmer Education