
Limmer Education

by Limmer Education
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
How do you approach NREMT questions? Let’s take a look at a practice question and walk through the process for answering it.
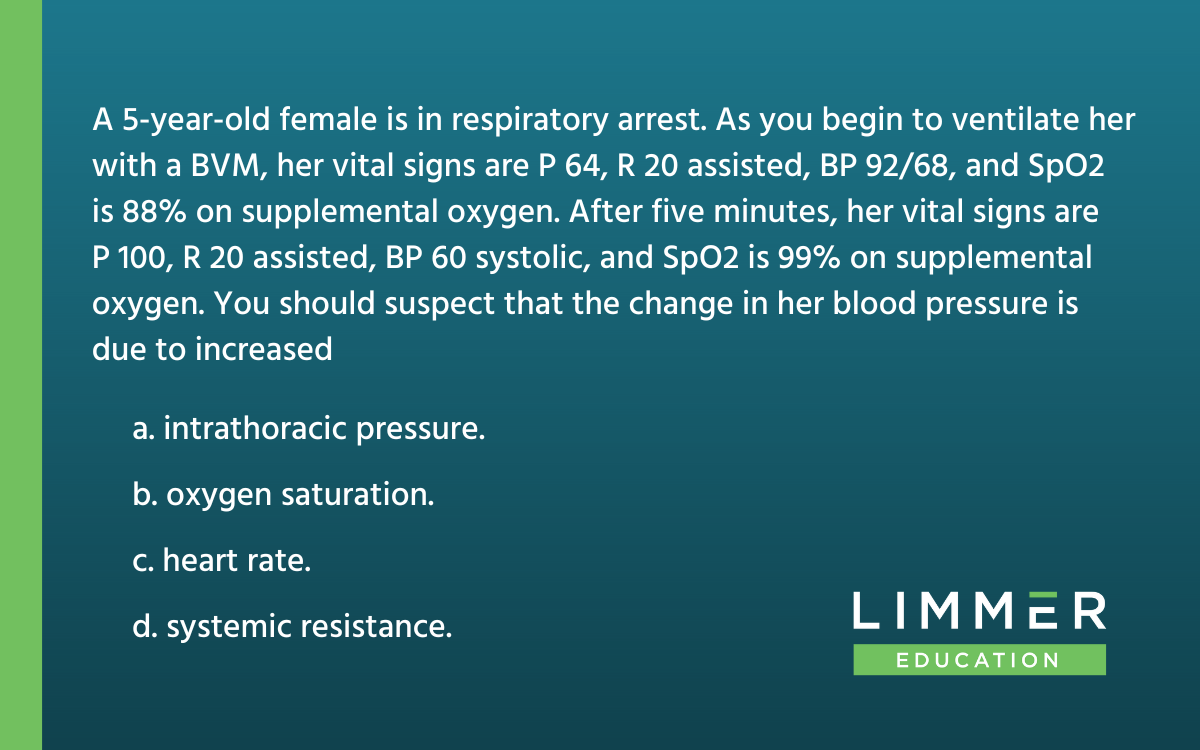
The first thing most people notice about this question is that it is dense with detail. Don’t let the details overwhelm you. Length has nothing to do with how difficult a question is.
There’s a reason for each piece of information in the question. After you read this question the first time, tell yourself, “OK, there’s a lot of information here. Let’s break it down.” Then re-read the question, pausing at each detail to reflect on what it means for the patient.
If you’re studying for the NREMT, get a piece of scratch paper and write notes. If you’re taking the NREMT, the exam center will give you a piece of paper or a little whiteboard to use. Not every question on the test is this dense, so don’t worry about taking extra time for this – there’s plenty of time.
What information is the first part of the question giving us?
She’s 5 years old. Think about how pediatric care might differ from adult care.
She’s in respiratory arrest, not respiratory distress.
Pulse is 64. Red flag. You should think of hypoxia and bradycardia.
Heart rate matches her age and condition.
Blood pressure is fine for her age.
SpO2 is 88%. Another red flag.
You started ventilating her with supplemental oxygen. After 5 minutes of ventilation, here’s how her vital signs changed:
Pulse went from 64 to 100.
Heart rate stayed the same, 20 assisted.
Systolic blood pressure dropped from 92 to 60.
SpO2 went from 88% to 99%.
What do those changes tell you? The changes in pulse and saturation tell you that the ventilation helped the hypoxia. That’s great, but now there’s a new problem: Her blood pressure dropped significantly.
Reading the last line of the question, we see that this is the heart of the question. Do you know what’s causing the change in blood pressure?
Now that we’ve taken the time to think through each detail in the question, we should be able to narrow down our answer choices pretty easily.
There are two ways to get a question right: You can know which answer choice is correct. Or you can know which answer choices are incorrect, and let the process of elimination lead you to the right one.
For this example, we’re going to rule out the incorrect answers first.
Heart Rate x Stroke Volume = Cardiac Output. If heart rate increases, cardiac output increases too. This usually helps, not hurts, blood pressure. So, it’s not heart rate.
This is pretty basic; hopefully you already knew this wasn’t the answer.
Have you ever heard of blood pressure tanking due to raised oxygen saturation? No, this is not something that happens to the body.
This is also pretty basic and should be an easy choice to exclude.
Cardiac Output x Vascular Resistance = Blood Pressure. Vascular resistance is also called systemic vascular resistance. If systemic resistance increases, it makes blood vessels smaller. That’s going to increase the pressure, not decrease it.
If you understand vascular tone, you know that this can’t be the answer. (If you don’t understand vascular tone, you will need to learn about it before taking the NREMT.)
Take a step back and look at what happened with this patient. You ventilated with a BVM, and the patient’s blood pressure dropped.
The BVM is only positive pressure ventilation. Through ventilation, you actually changed the intrathoracic pressure.
Normally, when someone takes a breath in and has a lot of breath come out, that change in pressure helps move blood through the inferior vena cava in the chest. The blood comes up and goes to the right atrium; changes in the positive and negative pressure help move blood through those other low-pressure vessels. But with ventilation, you’re not getting the change between positive and negative pressure. It’s all positive pressure. You’re reducing preload. The blood from those veins isn’t going back to the heart.
You can actually tank blood pressure by ventilating too aggressively. This is especially easy to do with pediatric patients. The answer here is increasing intrathoracic pressure.
All of Limmer Education’s products get routine updates based on AHA guidelines, new research and changing best practices. Try our PASS Apps for unrivaled NREMT prep for EMT, AEMT and paramedic. Or join EMTReview.com to get access to practice tests and live NREMT prep sessions with Dan Limmer!

Limmer Education

Dan Limmer, BS, NRP

Limmer Education
I really enjoy this tip Thank you alot 🙏 I'm a student nurse