
Limmer Education

by Limmer Education
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
When it comes to the National Registry, there may be no greater nook and cranny – and no topic that causes more stress – than pregnancy and OB questions. So let’s take a look at the pre-delivery and delivery emergencies you want to be familiar with before taking the NREMT.
You may have been told, "don’t delay delivery" but there are a few instances where you absolutely do want to prevent delivery. In these scenarios, your role is to keep the baby safe until you can get Mom to the appropriate hospital.
The most common pre-delivery emergencies you might encounter are placenta previa, placental abruption, and preeclampsia and eclampsia.
This is a condition where the placenta implants either totally or partially over the opening to the cervix. In the beginning of pregnancy, this doesn’t cause much of an issue. But it does get dangerous as the pregnancy goes on, past the halfway mark and into the last trimester. As more and more pressure is put on the placenta, the hallmark symptom of placenta previa starts to appear: painless, bright red vaginal bleeding.
Placental abruption, sometimes called abruptio placentae, is when the placenta prematurely separates from the uterine wall. This frequently, but not always, causes vaginal bleeding. But it almost always causes pain. Placental abruption is commonly seen when trauma occurs in the last trimester of pregnancy. It may also be seen during labor if the placenta prematurely separates from the uterine wall.
Expect abdominal pain, back pain, tenderness, and sometimes a feeling of cramping. This is a serious condition – transport as soon as possible.
Preeclampsia is the development of hypertension and protein in the urine. It frequently includes water retention and swelling.
Identifying preeclampsia from normal pregnancy symptoms can be tricky, especially because every pregnant patient presents differently. Ask your pregnant patients if they’ve had routine prenatal care. At these appointments, they get their blood pressure checked and have their urine dipstick tested for protein and sugar. Keep in mind, preeclampsia can develop at any time.
As preeclampsia continues, patients develop edema, have increased hypertension, and increased protein in the urine, and finally, seizures begin. That's when preeclampsia becomes eclampsia: when a preeclamptic patient has a seizure.
In the field, our common delivery emergencies are nuchal cord, prolapsed cord, breech baby and single-limb presenting baby.
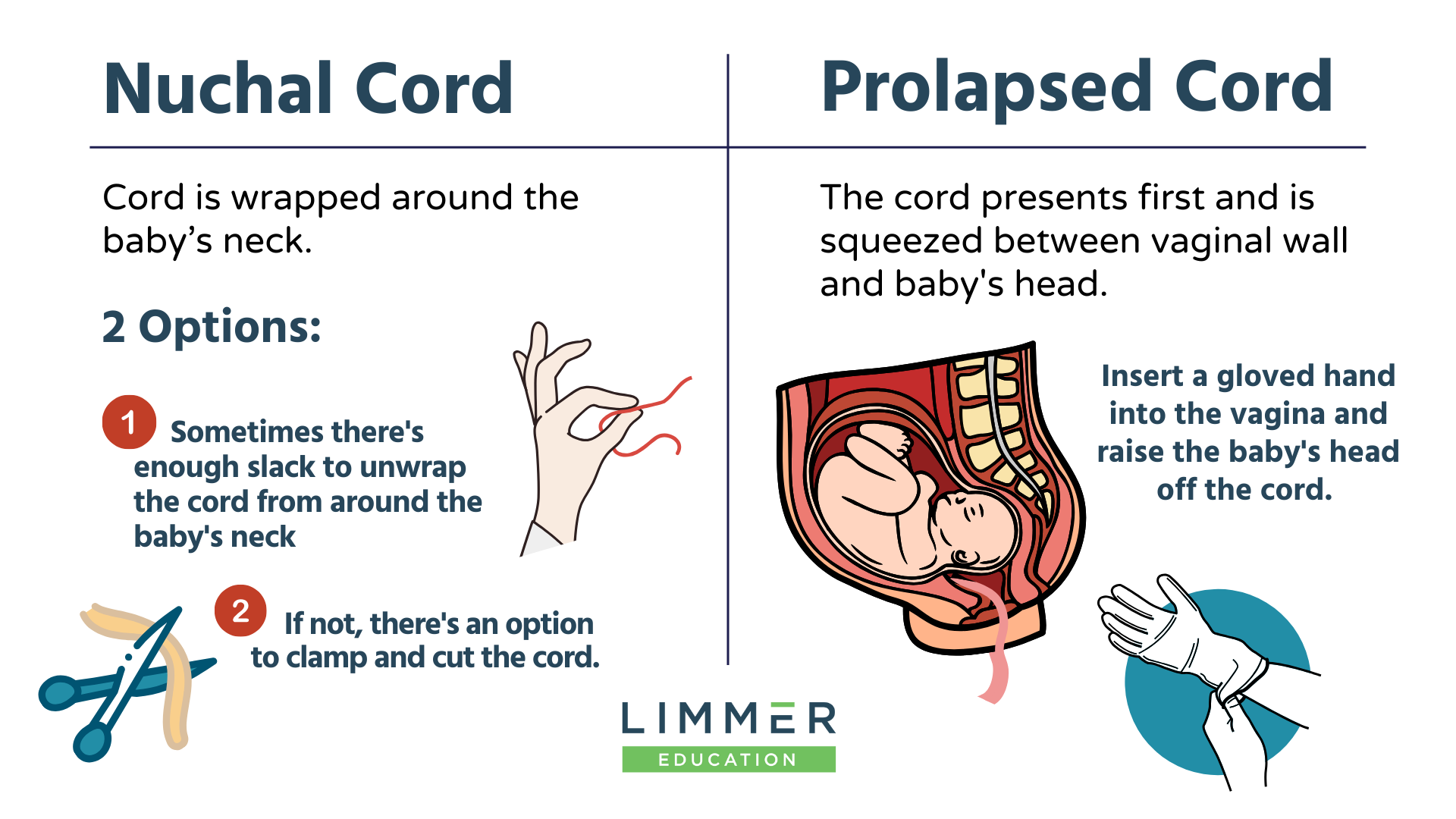
Imagine you’re delivering the baby, the head emerges, you look down, and the cord is wrapped around the baby's neck. This is nuchal cord.
You have two possibilities: Sometimes there’s enough slack that you can gently unwrap the cord from around the baby’s neck. That’s ideal. But if there’s not that much slack, you have the option to cut the cord. Use two clamps on the cord, and cut in between the clamps. Then continue the delivery.
What gives us a lot more trouble is prolapsed cord. This is when you see the umbilical cord as the presenting part. Instead of the baby’s crown, the umbilical cord is coming out first. EMS can’t deliver that.
With prolapsed cord, as the baby moves down through the birth canal, it puts so much pressure on the umbilical cord that the baby loses its oxygen supply. This is the one time you want to insert a gloved hand or fingers into the vagina and physically raise that baby’s head off the cord. You can also raise Mom's pelvis to move the baby back a little bit.
The most important thing here is to keep that baby’s head off the cord the entire trip to the hospital. Which hospital? The one that can handle a significant delivery emergency. You don’t want the baby moving any farther down the birth canal because it will cut off its own oxygen supply.
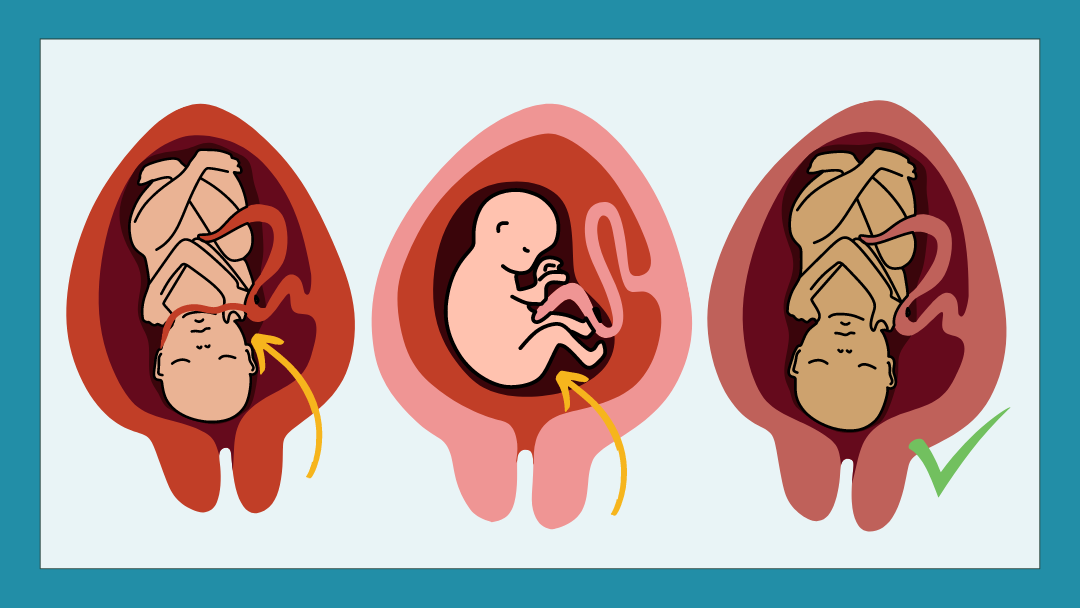
If the baby’s buttocks or both of the legs are presenting, that’s a breech delivery. We can do a breech delivery in the field, but if you’re able to transport Mom to the hospital – that’s the best option.
Single limb presentations are problematic. If one arm or one leg is presenting, you can't deliver. It’s not going to happen. So what do you do? You have to keep the baby viable. Raise Mom's pelvis to let gravity move the baby back, and transport to a hospital that can handle a significant delivery emergency.
You want to see the baby’s head. Mom should be having major contractions, then you’ll see some crowning, coach Mom through pushing if you can, and you’ll see baby’s head and shoulders emerge. This is called a cephalic delivery and it’s a beautiful thing.

Limmer Education

Dr. Bill Young

Limmer Education
Keep the information coming. Thank you!