
Dan Limmer, BS, NRP

by Limmer Education
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
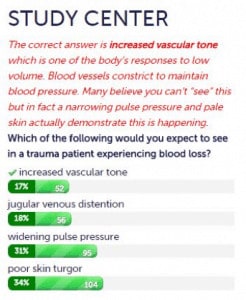
We put weekly poll questions on our EMTReview.com site. They are designed to challenge students or highlight important topics. On one recent pathophysiology question, we noticed that very few students got the correct answer. The answers they chose showed very little understanding of pathophysiology.
We probably don’t have to mention that one of the hallmarks of the current education standards is greater understanding—much of which is based on pathophysiology.
The stem was straightforward:
Which of the following would you expect to see in a trauma patient experiencing blood loss?
The distractors weren’t particularly challenging—some (widening pulse pressure and JVD) were actually opposites of what you would expect to see. Skin turgor can indicate volume depletion but this is a later sign. Increased vascular tone (chosen the least) is an early and predictable reaction to blood loss. It wasn’t a difficult question.
There are a lot of reasons students could get this wrong. They may have read too quickly or just picked any choice so they could see the correct answer. But what about the students who tried and got it wrong? Some of these students didn’t get the pathophysiology they needed in class.
This may be because it wasn’t taught in depth or terms like “vascular tone” weren’t used—or weren’t used enough. Students need to know different terms (constriction, resistance and tone) for the same concept to be optimally prepared for the NREMT.
Some educators might be saying, “It isn’t my fault if the students didn’t learn it. I taught it.”
But hold on - sure, the student might have glossed over vascular tone in the depths of that initial pathophysiology presentation. But what about the cardiology presentation, the anaphylaxis presentation, the sepsis presentation and the shock presentation? (Notice we didn’t call them lectures because we hope there are some active components to the classes.) The concept of vascular tone applies in each and every one of those topics too. There is no reason an EMT should get out of class without knowing this concept.
Try giving this question to your students at some point in the upcoming semester to test their knowledge of simple pathophysiology. And while you are preparing for this semester, plan on integrating a bit more pathophysiology.

Dan Limmer, BS, NRP

Dan Limmer, BS, NRP

Dan Limmer, BS, NRP
I agree with Melissa. The wording will throw students. Peripheral vasoconstriction/dilation are terms I typically use. Helps them understand skin condition/color. From my perspective, test writers have a tendency to write a question that is based on documentation that they themselves studied from or achieved their knowledge from. Don't get me wrong, I understand vascular tone but, typically wouldn't utilize that wording.
I do think there is a problem with test writing. If we want our students to truly understand what is wrong with the patient and how to then apply management, the focus on test taking shouldn't be on being so technical on vocabulary. Get to the point. We should feel comfortable that they can identify shock practically.
I'm with Alex on this one, though I had some of Melissa's concerns over instructor vocabulary given many instructors do have near zero training in these areas themselves. That lack of training within the instructor cadre only speaks louder to the bottom line which is that one cannot effectively teach PATHOphysiology until the student has an understanding of PHYSIOLOGY. Even at the EMT level (which should only be a free-standing level for areas that cannot support anything else), there needs to be pre-requisite knowledge before you go into the professional training. Requiring a full year of A&P with lab prior to paramedic entry may likely go down as the best change we've ever made to our program.
This could also be a reflection of rote memorization or restricted range of instructor vocabulary in teaching. Students may have recognized - perhaps even understood the concept of the correct response if it was phrased "vasoconstriction" but instructors may not be explaining concepts multiple ways. Many EMS instructors are self-taught in physiology, pathophysiology (and pharmacology, etc.) and may not have used multiple resources in doing so. Doing a "think aloud" with students who responded correctly and those who didn't could give more information on whether this is truly a lack of understanding of shock, or unfamiliar (although correct) terminology.
Until everyone starts treating prehospital care as a stand alone profession that requires A&P, Physiology, Pharmacology Psychology and a few other select courses as an entry point. The system today will remain fragmented and in disarray.