
Dr. Bill Young

by Dan Limmer, BS, NRP
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
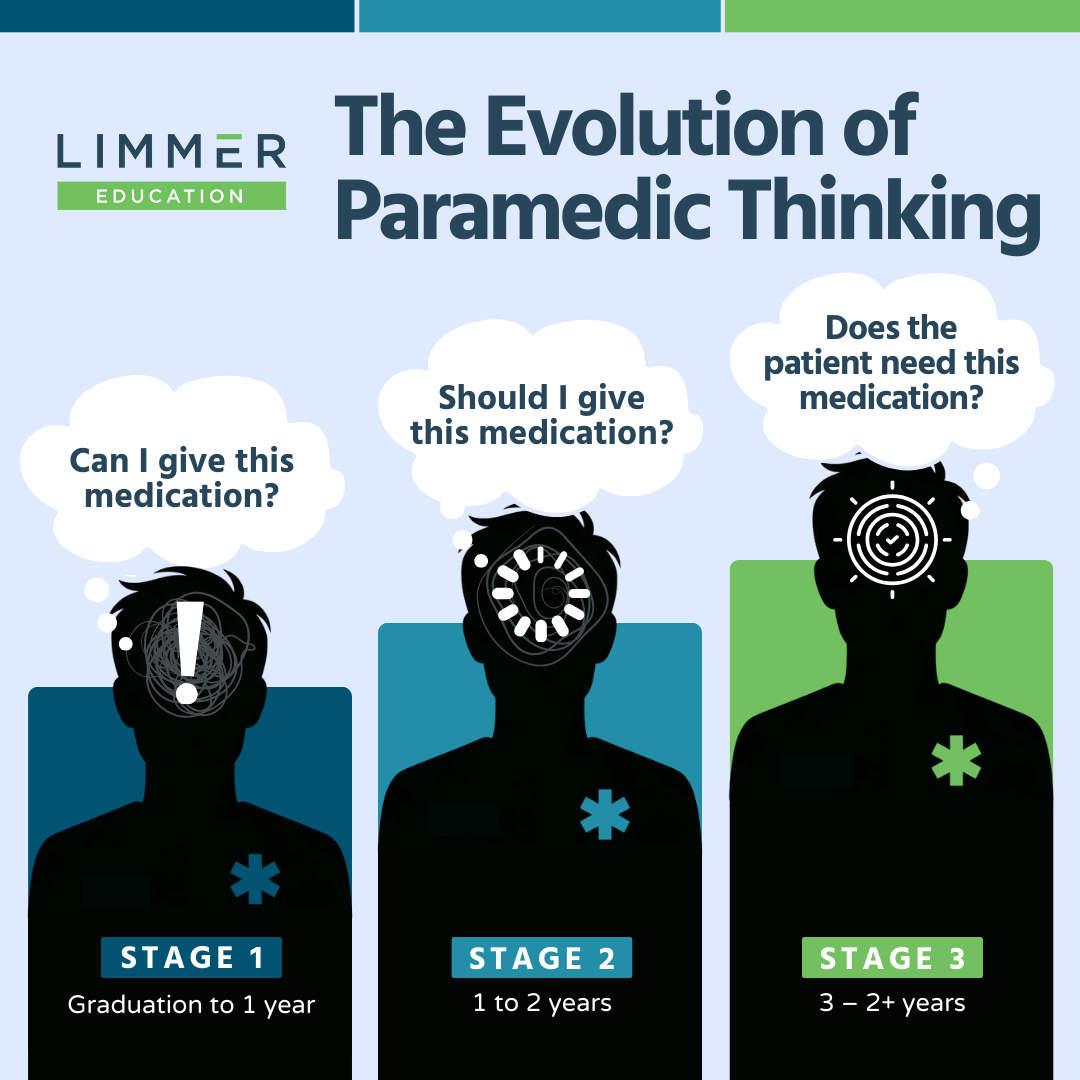
As long as there have been paramedics, there has been an evolution of paramedic thinking and judgment. The clinical parameters that shape that judgment haven’t changed a lot over the years. Pathophysiology and disease don’t change a lot. But the way paramedics think when they leave class through the 3-5 year mark does change a lot.
From once being a young paramedic to having precepted and worked with many different paramedics over the years, I present to you the Evolution of Paramedic Thinking.
Also called “I’m Going to Give This Medication” or “But It’s in My Protocols…”
The new paramedic has a big toolbox at their disposal. Their goal is to use it. Often. Thinking is centered around themselves first and the patient second. The thinking here is “Can I give this medication?” Each call is an opportunity to pull something out of the drug box and use it. Administering medications and performing skills like chest decompression create stories and experiences. It feels good. It is excitement driven. Actual clinical decision making is limited and not the primary focus.
As the paramedic gets out of the excitement-driven first year, some clinical thinking begins to evolve. Reality sets in and there may be a crisis in confidence that slows down the previously careening skill and medication train. A bad experience or two sometimes fuels this change of heart. This paramedic thing may be more challenging than they originally thought.
The next step causes the paramedic to ask themselves, “Should I give this medication?” It brings an attempt to balance the prior stage with clinical thinking—although not as well as happens in the next stage.
While the paramedic may still be a distance from a clinical pinnacle, this shift is the most significant—and the most clinically focused. The experience of the first two years coalesces and the focus shifts significantly from the self to the patient. The paramedic has refreshed their NRP certification.
Experience isn’t the only factor here. How an agency values critical thinking and implements quality improvement (culture) is foundational to the development of a paramedic. The medical director can provide a positive influence here.
Confidence plays a role in thinking. Positive experiences over time, support and guidance through the tough times when confidence is tested, and positive role modeling helps form a confident and clinically relevant provider.
Disillusion is the negative side of the equation. This is a make-or-break point where clinical thinking can thrive—or not. Culture plays a role here as a paramedic balances the realities of the job over time with quality patient care.
Every paramedic’s story is different, and your mileage may vary. Some paramedics “get it” from day one while others relive their first year every year for an entire career. What is your experience as a new medic? Your experience as a preceptor or partner of a new medic? We’d love to hear about it in the comments.

Dr. Bill Young

Limmer Education