Trusted Education for the Future of EMS
NREMT prep and classroom solutions that build better providers.
The Limmer Advantage







Made by NREMT Experts
Clinical Depth
From Class to Field and Beyond




NREMT Success
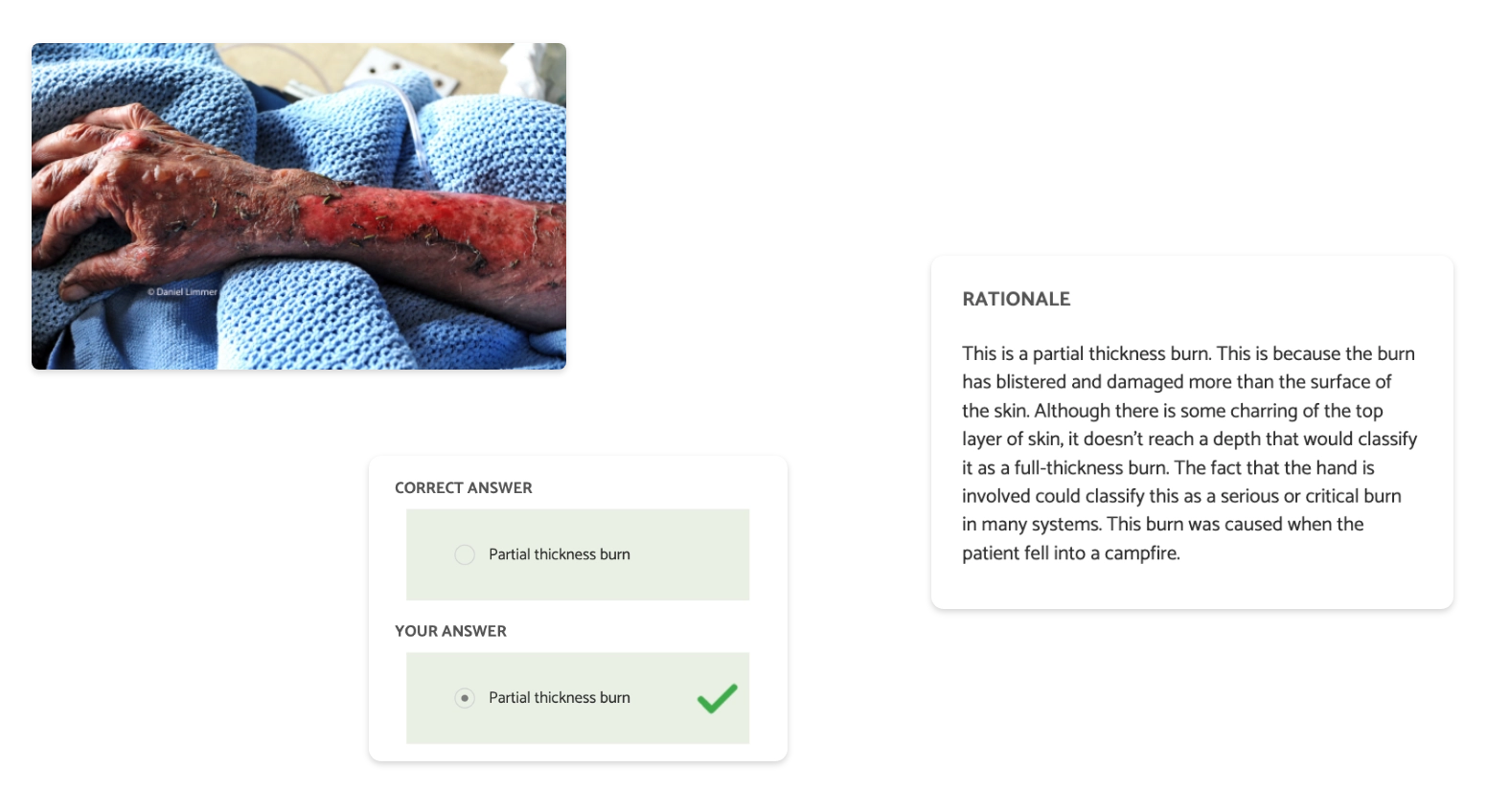
Help students succeed on their exams. Our apps focus on critical thinking, pattern recognition and pathophysiology.
Get startedAfter using your products and learning how to attack and understand questions I felt more confident than ever. The material you offer is amazing! It helped me to finally pass my NREMT! – Trevor D.
Educator Tools
We’re here to help you create a more dynamic, inspiring, and productive classroom.
Get startedI recommend Limmer resources to all my students. The pass rates are much higher and students have shown to be more efficient and effective in the field as a result. – Scott Stephens
Knowledge & Application
Our NREMT remediation courses help users pass… and give them relevant, deep understanding. 24-hr. EMT / 36-hr. AEMT
Get startedMy saving grace! I completed your online remediation and went in to take my third attempt and passed! Thank you!! – Sidney F.
CAPCE Approved
The 7 Things EMS podcast provides fluff-free, boredom-free CE for a variety of topics, from education to toxicology.
Get startedThank you for this podcast. I have learned so much and love that I can get CE for listening. – Julie R.

Find Your Match
We have a wide variety of apps for all different stages of your EMS education.
Use our product finderFrom our EMS Articles
Loved by EMS Students, Educators and Institutions
-
-
I failed the NREMT 3 times, so I decided to purchase the remedial training and watching his videos and taking the practice test on each topic 3 times really help me understand the concepts and what to look out for in the NREMT test... Limmer Ed is the real deal. I passed on my 4th attempt.
David R.EMT -
With the help Limmer apps I was able to understand the concepts and know the material, not just memorize it. I would highly recommend your products to anyone looking to pass their NREMT or just get a better understanding of how to become a better EMT.
Chris T.EMT
-
-
-
As a program director I buy bundles at a time and the price value is great. The material has been instrumental in preparing my students for the NREMT exam... The array of apps available, the ease of use on a mobile device and computer, the price, the customer support, and overall quality is top notch. I will continue to use the LC-Ready family of apps for years to come.
Juston ArnoneChief of Medical Services -
You guys have the absolute BEST customer service!
Cindy W.EMT-P Dept. Head
-
-
-
On my third and final attempt at the NREMT exam I am relieved to say that I am now NREMT certified! Preparing for this exam brought with it so much stress, which was good in part, as I was truly ill-prepared to work in EMS. This [EMT Remediation] course was logical and challenging, teaching me valuable skills and knowledge. However, most importantly I learned how to think more critically and calculated when faced with a patient.
MaxEMT -
I studied this for 2 weeks before taking the NREMT... the questions are very alike! And I found out that I'm an EMT!! Best app ever!!!
Sean D.EMT
-