
Dr. Bill Young

by Limmer Education
Our articles are read by an automated voice. We offer the option to listen to our articles as soon as they are published to enhance accessibility. Issues? Please let us know using the contact form.
One of the biggest issues we hear about when talking to our students and educators, after NREMT exam anxiety, is confusion about the patient assessment process for EMTs.
The EMT assessment has changed quite a bit over the years, and a brief history may help to understand why it's such a concern today.
Pre-1994 EMT-A curriculum used a primary assessment and secondary assessment approach.
The 1994 EMT-B curriculum changed the terms and structure quite a bit. Initial assessments and focused assessments, with rapid options, became the new terms and processes. The big issue was that the EMT-B curriculum didn’t cover anything in detail if the EMT couldn’t do anything about a condition. This left gaps in both knowledge and assessment.
Then again in 2009, education standards went back to a primary and secondary assessment concept. However, it didn’t provide the detailed steps of a curriculum. Pathophysiology and rapidly expanding treatment options made assessment even more important—but it's taking us a while to shed the 1994 terminology and philosophy.
This brings us to the 2020s, where, because of the rapidly expanding toolbox, EMTs need in-depth assessment skills—yet we struggle with lingering terminology (and attitudes) of 1994.
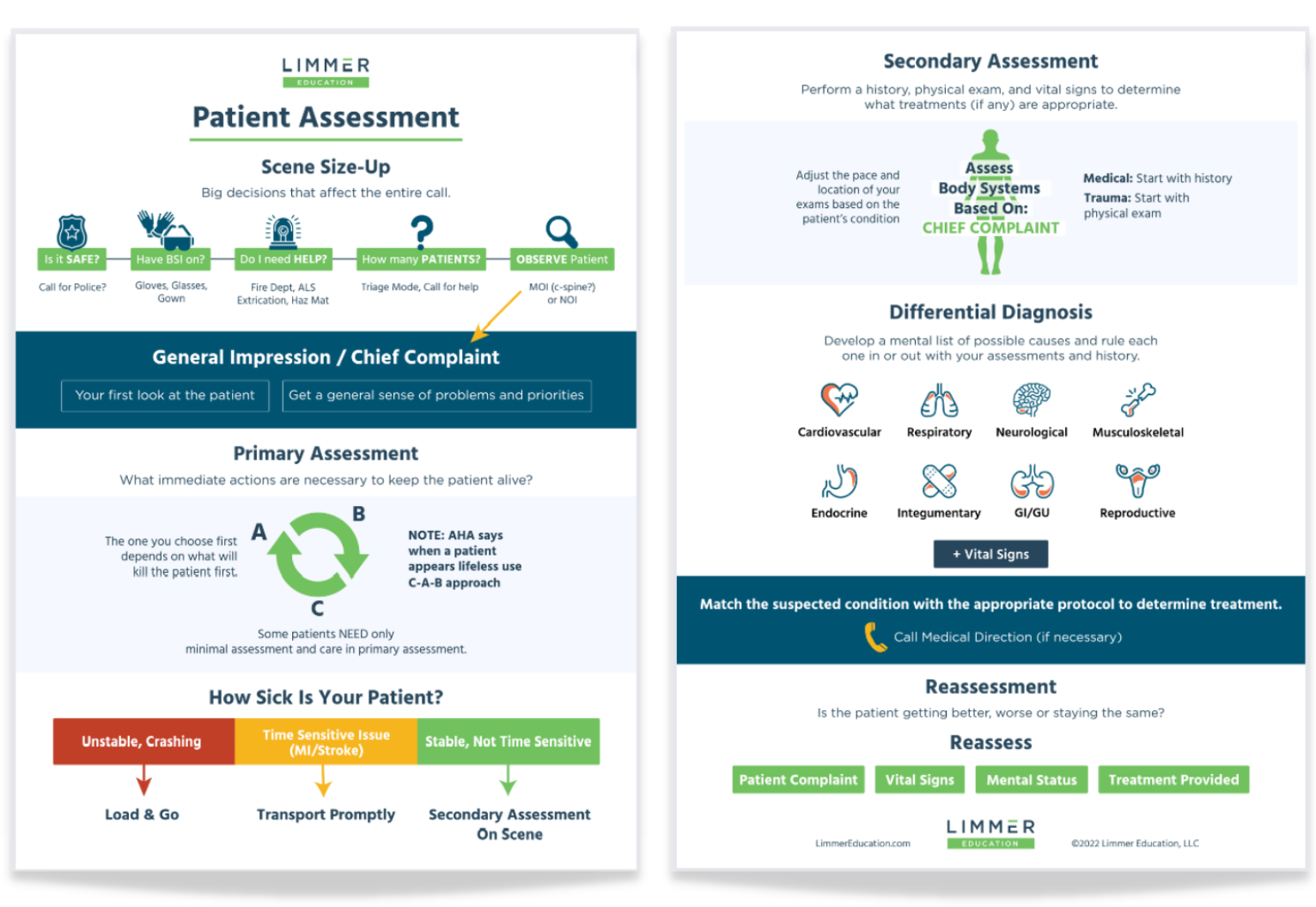
The mantras of the old need to make way for a more mature, efficient, and thought-based process. For this reason, we created the Patient Assessment Flowchart.
A few things about the new flowchart:
The scene size-up has two distinctly different phases: the safety and resource phase and the approach to the patient phase. First, make sure the scene is safe and buttoned down. Then, look toward the patient for important clues. This method provides a seamless flow into the primary assessment.
The primary assessment is non-linear, demonstrated by the circular graphic. What do we do first in the primary assessment? Fix the thing that is likely to kill the patient first.
We’ve added a continuum to show that there are a wide variety of patient situations when it comes to making priority decisions. And there are multiple factors that come into play when figuring out how fast or slow you need to proceed in the rest of the assessment.
There is a real difference between medical and trauma patients—but not as significant as it was once taught. In the trauma patient, we examine multiple body systems in a hands-on exam.
SAMPLE and OPQRST are much less prominent. This is because they've become a mindless crutch for students and educators. We need to return them to the place they belong—as mnemonics—for when we want to make sure we’ve covered the basics. They are not the primary driver for the history.
So what's the driver for history and physical exam if SAMPLE and OPQRST aren’t? Body system exams. We need to know to look for JVD and pedal edema routinely in the cardiac and respiratory patient. We must ask about orthopnea, weight gain, and dyspnea on exertion. We would find none of this if we only used OPQRST and SAMPLE. Pathophysiology allows us to understand more and to know what to ask.
In spite of the lack of the assessment terminology we are used to, this flowchart still aligns very well with the NREMT skill sheets for both medical and trauma patients.
It's time to get rid of old, confusing mantras and make patient assessment effective, modern, thought-based, and intuitive.
Please feel free to share this with your classes and agencies. We’ve also created a video overview of the patient assessment flowchart, which you can watch below. We’d love your feedback.

Dr. Bill Young

Mike Miller

Limmer Education
LOVE THIS. Ill be sharing with my service immediately
This makes so much sense to me, and is so less stilted than the existing SAMPLE OPQRST terminology. Thanks also for giving us the history; I was confused by the older lingo. When you say "we created the Patient Assessment Flowchart [for the 2020's]," does this have any support from national standard-setting bodies? It would be really nice to see this become a national curricular standard, rather than a guide limited to limmereducation.com. (I'm actually OK with SAMPLE; it's OPQRST that I find awkward at best and misleading at worst).
Hi James--thank you for the kind words and an excellent question.
While the NREMT has taken down their patient assessment skill sheets at the EMT level, I think you'll find that these actually match up pretty well. I had similar thoughts when we put this piece together.
But then I thought, at what point do we (EMS as a profession) leave a lockstep approach for assessment and go with more goal-oriented assessments? The processes taught in medicine and other allied health professions don't rely on national accrediting bodies to provide a particular set of steps. They combine A&P, pathophysiology, assessment, intuition, etc. into a successful end result.
I don't believe our students will see a lot of questions like, "What is the line after vital signs on the skill sheet?" (ok--being a little dramatic here). What they ask--and what our students need--is to be able to identify criticality, have appropriate priorities, and have the assessment lead to appropriate patient management.
It is just very hard for us to let go of the old EMT-B attitude.
Thanks again for writing. Dan
This is great knowledge and information for the EMS. I appreciate your support while preparing for the NREMT Exam on April6/21. Thanks a lot Dan, a great job well done!
Better study tools=less stress for my students. Limmer is the clear winner!
Awesome video I'm going to show this to our EMT class.
[…] Dan’s blog article and pdf can be found at:https://limmereducation.com/patient-assessment-2019/ […]